Trồng răng Implant - phương pháp trồng răng hoàn hảo nhất
CÁC DỊCH VỤ TẠI NHA KHOA NHÂN TÂM

Dịch vụ phục hình răng sứ trên Implant
Sau khi đã cấy ghép trụ implant, khách hàng sẽ được đặt mão sứ với mục đích hoàn thành một chiếc răng mới chắc chắn như răng thật, đảm bảo được chức năng ăn nhai cũng như tính thẩm mỹ.

Dịch vụ trồng răng Implant tức thì
Trồng răng Implant tức thì ngay sau khi mất răng là phương pháp kết hợp cả nhổ răng và trồng răng Implant trong cùng một lần phẫu thuật được ứng dụng phổ biến hơn nhờ nhiều ưu điểm nổi trội

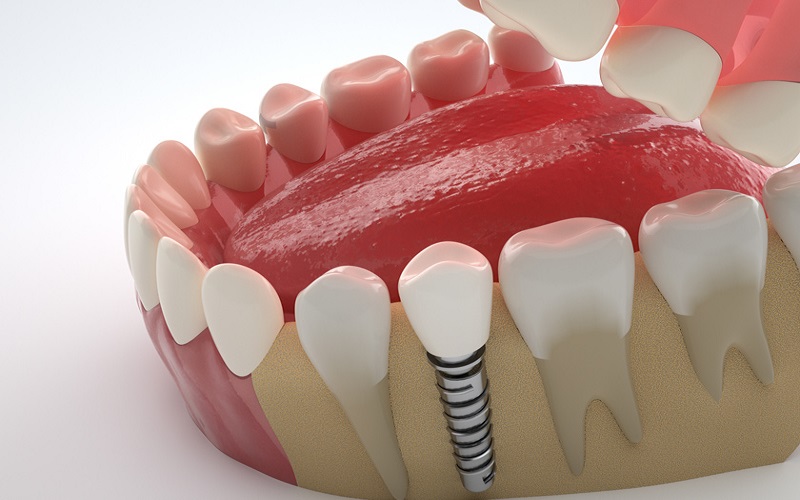
Trồng răng Implant thay thế một vài răng
Trồng răng Implant thay thế một vài răng là giải pháp cấy ghép trụ implant (2 chân trở lên) vào trong xương hàm thay thế chân răng đã mất, gắn mão sứ khôi phục lại tính thẩm mỹ và chức năng của răng
Ưu điểm trồng răng Implant đơn lẻ
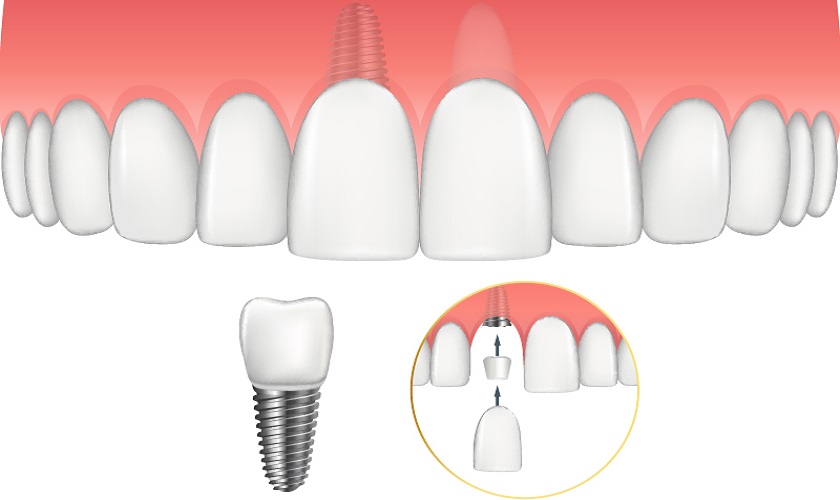
Trồng răng implant là giải pháp phục hồi răng mất an toàn và hiệu quả lâu dài. Phương pháp này cấy một trụ titanium vào xương hàm để thay thế chân răng đã mất, sau đó phục hình mão răng sứ lên trên

Kỹ thuật trồng răng Implant All on 4
Trồng răng Implant All on 4 là một giải pháp phục hình răng tân tiến bậc nhất hiện nay, giúp người mất răng toàn hàm khôi phục lại cả vẻ đẹp thẩm mỹ lẫn chức năng ăn nhai với chi phí tiết kiệm
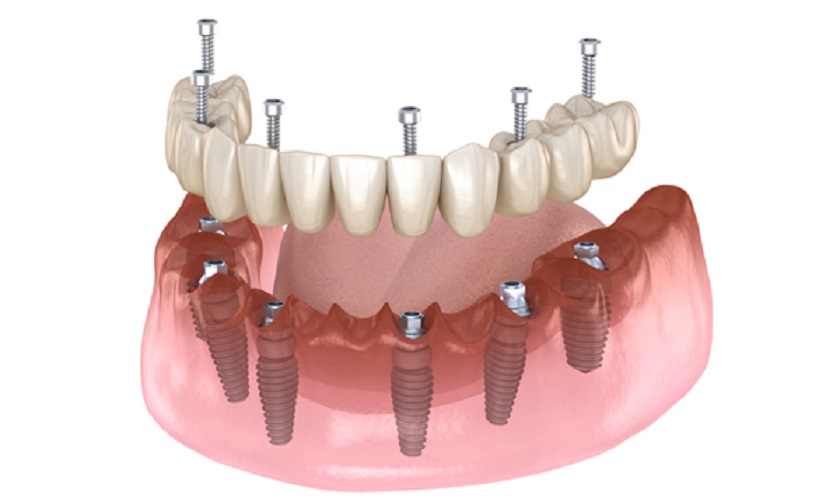
Kỹ thuật trồng răng Implant All on 6
Trồng răng Implant All on – 6 được xem như “vị cứu tinh” với người bị mất răng toàn hàm do tuổi tác, di truyền, bẩm sinh hoặc do chấn thương, tai nạn,… với chi phí tiết kiệm mà vô cùng hiệu quả
CHUYÊN MỤC IMPLANT NHA KHOA
TRỒNG RĂNG CHO NGƯỜI KHÔNG RĂNG BẨM SINH
NÂNG XOANG - GHÉP XƯƠNG TRONG IMPLANT
GHÉP NƯỚU & TẠO HÌNH THẨM MỸ NƯỚU
CÔNG NGHỆ HIỆN ĐẠI TRONG CẤY GHÉP RĂNG IMPLANT
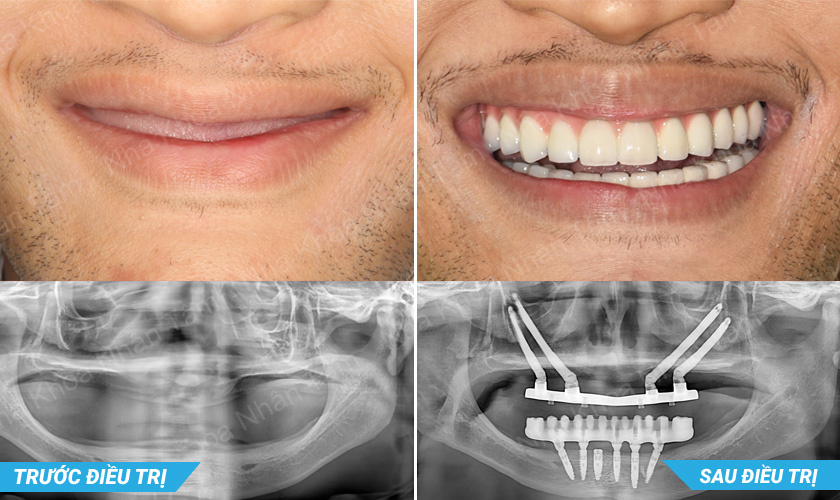
HÌNH ẢNH MỘT SỐ CA ĐIỀU TRỊ IMPLANT ĐIỂN HÌNH
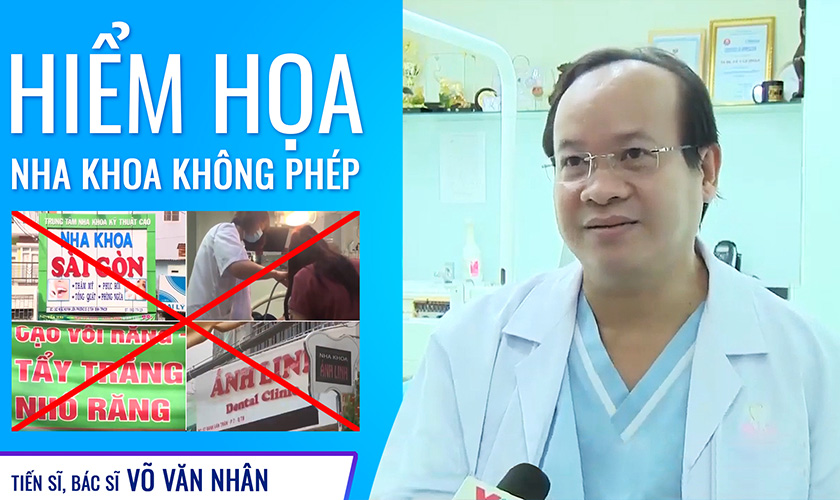
Tiến sĩ, Bác sĩ Võ Văn Nhân
Là người tiên phong trong các kỹ thuật phức tạp trong chuyên ngành Implant như: Ghép xương tự thân 3 chiều (2011), ghép xương khe hở huyệt răng để cấy ghép Implant cho bệnh nhân khe hở môi (2012), khâu vá màng xoang bị thủng lớn (2012), phẫu thuật dời thần kinh ổ răng dưới và cấy ghép Implant đồng thời (2013) và cấy ghép Implant xương gò má cải tiến (zygomatic Implant) (2014), cấy ghép Implant xương gò má cải tiến kết hợp với dời thần kinh ổ răng dưới và cấy ghép Implant đồng thời trong phục hồi răng cho bệnh nhân loạn sản ngoại bì không răng bẩm sinh (2016), ứng dụng tế bào gốc trong ghép xương và cấy ghép Implant (2017).
Chuyên gia cấy ghép Implant
Bác sĩ Việt Nam đầu tiên áp dụng thành công Robot định vị trong cấy ghép răng Implant.
Báo cáo viên khoa học
Báo cáo viên tại các diễn đàn khoa học trong nước và quốc tế, đạt được nhiều giải thưởng nghiên cứu khoa học danh giá.
Giảng viên ĐH Y Dược
Giảng viên Implant tại các trường Đại học Y Dược TP.HCM, Đại học Y Hà Nội, Đại học Quốc tế Hồng Bàng,…
Công trình nghiên cứu
Có nhiều bài báo được xuất bản trong và ngoài nước về lĩnh vực nâng xoang, ghép xương và cấy ghép Implant trong những tình huống phức tạp.

THƯ VIỆN VIDEO